Active Snakebite
Snakebites are medical emergencies! Once you are safe and stable, please join the National Snakebite Support Facebook group.
Disclaimer: Information shared is for educational purposes and there is no doctor-patient relationship established by joining or conversing with NSS experts or staff.
Please note, this is a private Facebook group. You will be prompted to answer entry questions. Membership will be denied for inaccurate or incomplete responses.
ACTIVE SNAKEBITES: Please answer ACTIVE BITE to the first question to expedite membership.
GENERAL ENTRY: Please answer all questions with the appropriate responses to enter the group.
Snakebite Management for Humans
NSS Pre-Hospital Management
The most important steps following a bite are:
Arrange to get to the hospital as quickly as possible. That may mean calling a friend or 911. Definitely call 911 for any serious symptoms. Do not drive yourself.
Remove any constrictive clothing and jewelry.
Elevate the affected extremity (please see the article explaining why we elevate). Absolutely DO NOT place the affected extremity below heart level.
Take a picture of the snake IF YOU CAN DO IT QUICKLY AND SAFELY. It is helpful but not necessary. DO NOT bring the snake, whether dead or alive.
DO NOT do any of the following: tourniquets, lymphatic bandage, pressure immobilization, cut and suck, extraction device, electrical stimulation, packing the extremity in ice.
NSS In-Hospital Management
The most important steps to be taken in-hospital:
Keep the affected extremity elevated.
Make sure they check the following laboratory tests: CBC, BMP, PT/INR, Fibrinogen, CK.
Ask them what their indications for antivenom are, and make sure they are consistent with what we have mentioned here:
Significant or progressive local tissue damage; e.g., tenderness and swelling that crosses one major joint, hemorrhagic bleb
Hematologic toxicity; e.g., PT >15s, fibrinogen <150mg/dL, platelets <150K/µL
Systemic toxicity; e.g., hypotension, airway swelling, neurological toxicity
If you do not feel you're getting appropriate care, advocate for yourself. Request they involve an expert. If necessary, request transfer to a more appropriate facility.
Do not agree to prophylactic antibiotics or prophylactic surgical intervention.
Click for the BMC Emergency Medicine Unified Treatment Algorithm for the Management of Crotaline Snakebites in the United Statesand flowchart for your physician to review.
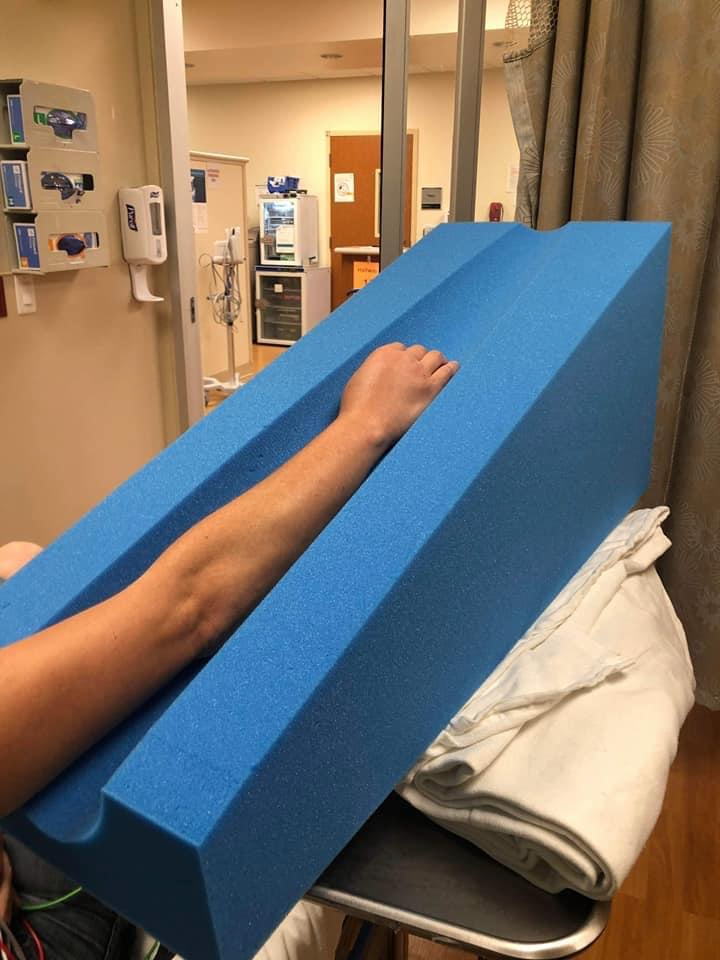
Example of proper leg elevation
Example of proper arm elevation
-
Written by Dr. Spencer Greene
When determining how to position the affected extremity following a snakebite, there are two things to consider: (1) the type of snake, and (2) whether you’re already at the hospital or still in the pre-hospital environment.
Experts agree that crotalid (copperhead, cottonmouth, rattlesnake) envenomations should be ELEVATED in the hospital. Elevate the extremity at least 45° (ideally at least 60°) without allowing the knee or elbow to bend. It’s one of the first recommendations in the unified treatment algorithm for the management of crotaline snakebite in the U.S.
Pre-hospital positioning is a little controversial. Some people recommend keeping the affected extremity at heart level because they fear that elevation will increase the systemic absorption of the venom. Dr. Spencer Greene recommends early and aggressive elevation, because the volume of venom is so insignificant that elevation is unlikely to make a difference in absorption. On the other hand, the volume of fluids that accumulate in the affected extremity is significant, and elevation will reduce that swelling. He reports seeing dramatic improvement within 30 minutes of elevation.
The affected extremity should never be placed below heart level. This will increase the swelling and hydrostatic pressures that lead to tissue injury.
Coral snake envenomations do not cause significant swelling, and we recommend patients placing the affected extremity in whatever position is most comfortable.
You can read Dr. Greene’s snakebite positioning article here.
Snakebite Management for Dogs and cats
NSS Veterinary Pre-Hospital Management
The most important steps following a bite are:
Distance your pet and yourself from the snake. Do NOT endanger yourself by getting within striking range of the snake in order to catch your pet. If you get bitten, you will not be able to help your pet.
If you can do so safely, take a photo of the snake. ID is not required for proper treatment.
Do not attempt to capture, kill, or transport the snake. Interacting with a defensive snake increases the likelihood of you being envenomated.
Remove collars, leashes, harnesses or anything constricting in areas where the bite or swelling is present.
Avoid excitement or strenuous activity to the best of your ability.
Do not administer any medication, especially NSAIDs (Carprofen, Rimadyl, Miloxicam) as these increase bleeding tendencies and may cause kidney injury.
Head immediately to the emergency vet. Call ahead to confirm antivenom is stocked. Snakebites are a medical emergency and there are NO effective home remedies.
NSS Veterinary In-Hospital Management
The most important steps to be taken in hospital are:
Discuss treatment plan with your vet and reference the In-Hospital Management guide.
Labs are necessary to monitor the progression or regression of the venom effect. Labs to request will be CBC, chemistry, pcv/ts to assess for hemolysis, PT/PTT, and a blood film to count/confirm platelets and look for echinocytes.
Antivenom, if warranted, non-NSAIDs pain medication, and IV fluids (not subcutaneous fluids) are the indicated for envenomation.
Antivenom is most effective directly following envenomation, but can still provide benefit several days after the bite if venom effects are present.
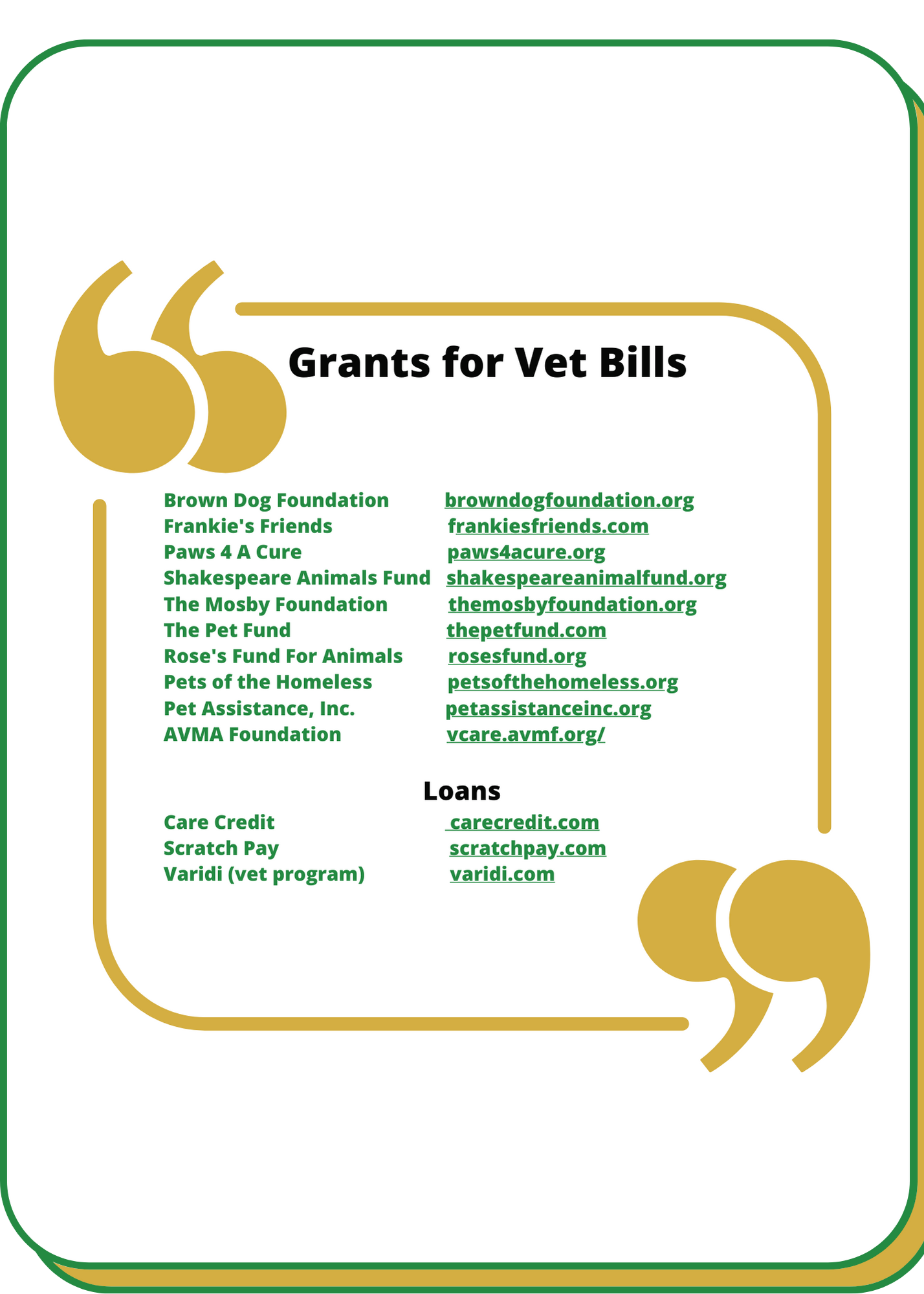
Scratch Pay and Care Credit are the most common vet funding resources.
Download the NSS Veterinary Pit Viper Management flowchart and NSS Veterinary Supplemental Information for Pit Viper Management for Envenomations here for your veteranian.